Precision Medicine: The Pioneers and How DNA Origami Could Take It to the Next Level
Precision medicine, an approach that tailors medical treatments to individual patient characteristics, has taken significant strides in recent years. Among the most prominent developments are Chimeric Antigen Receptor T-cell (CAR-T) therapies, Antibody-Drug Conjugates (ADCs), and broader Immunotherapies. These treatments have dramatically altered the medical landscape, offering newfound hope for patients with previously intractable conditions. Yet, there remains an untapped potential in these therapies—potential that DNA origami may help unlock. This blog post aims to delve into the nuances of these technologies and shed light on how DNA origami could revolutionize the future of precision medicine.
CAR-T Therapies: Personalized Cellular Attacks on Cancer
Let’s begin with CAR-T therapies. In essence, these treatments modify a patient’s own T-cells to recognize and attack specific cancer cells. Think of it as training your immune cells to become specialized cancer-hunters. CAR-T therapies have shown incredible promise in treating certain blood cancers, leading to miraculous recoveries that were previously unimaginable.
CAR-T stands for Chimeric Antigen Receptor T-cell. The term “chimeric” refers to the artificially engineered nature of these cells. In essence, scientists modify regular T-cells to express a specialized receptor—the Chimeric Antigen Receptor (CAR)—that can recognize a specific protein found on the surface of cancer cells. The result is a T-cell with an enhanced ability to seek and destroy cancer cells.
The process begins by collecting T-cells from the patient’s blood. These cells are then sent to a lab, where they are genetically engineered to express the CAR that targets cancer cells. Currently, cells are modified through the use of viral vectors, which is current limitation of the system. After modification, these T-cells are multiplied in the lab to create a large army of CAR-T cells, which are then infused back into the patient.
Once reintroduced into the patient’s bloodstream, these engineered CAR-T cells begin their search for cancer cells. When they find a cancer cell with the target protein, the CAR-T cells bind to it and initiate a sequence of events that lead to the destruction of the cancer cell. This process includes both direct killing by the CAR-T cell as well as signaling other immune cells to join the attack.
The Challenge
However, CAR-T therapies are not without their complications. They require extracting cells from the patient, modifying them in a lab, and then reintroducing them. This process is both time-consuming and costly. Additionally, there’s the risk of severe side effects like cytokine release syndrome.
- Side Effects: One significant concern is the possibility of “cytokine release syndrome,” a severe inflammatory response caused by the rapid activation of CAR-T cells that are created by viral vectors.
- Cost and Accessibility: The personalized nature of CAR-T therapy makes it expensive and time-consuming, limiting its availability.
- Manufacturing: Using viral vectors for gene therapies like CAR-T is a complex and resource-intensive process that requires specialized facilities and stringent quality controls. The need for high purity, safety, and efficacy, coupled with scalability challenges, makes the production of viral vectors one of the most critical bottlenecks in advancing gene-based treatments.
Antibody-Drug Conjugates (ADCs): The Sniper Rifles of Medicine
ADCs can be thought of as sniper rifles in medical treatment. They utilize the targeting capability of antibodies to deliver a toxic payload directly to a cancer cell, sparing healthy cells. This approach significantly improves the therapeutic index of traditional chemotherapies. Antibody-Drug Conjugates (ADCs) represent a promising avenue in precision medicine, aiming to combine the specificity of antibodies with the potency of cytotoxic drugs.
The Challenge
ADCs are not without hurdles.
- Payload Capacity: Ensuring sufficient drug delivery to maximize therapeutic effect while minimizing side effects.
- Combination Therapies: Limited development in combining ADCs with other treatments, which restricts synergistic treatment possibilities.
- Stability Concerns: ADCs can face stability issues during storage and in circulation, which can affect their efficacy.
- Patient Variability: Differences in patient responses and emerging resistance mechanisms can diminish the effectiveness of ADCs.
Immunotherapy: Awakening the Immune System
Immunotherapy is a transformative approach in the battle against cancer, leveraging the body’s immune system to identify and combat malignancies. Rather than directly targeting cancer cells, it amplifies or modulates the immune response to attack the disease. One groundbreaking example is the use of checkpoint inhibitors, such as pembrolizumab and nivolumab, which block proteins that prevent T cells from killing cancer cells.
Another innovative strategy is the employment of bi-specific T-cell engaging (BiTE) antibodies. These molecules can simultaneously bind to cancer cells and T cells, effectively bringing them into close proximity and facilitating the destruction of the tumor. Additionally, CAR-T cell therapies, which involve engineering a patient’s T cells to target specific cancer antigens, have shown immense promise, particularly in blood cancers.
Through these modalities and more, immunotherapy continues to reshape the landscape of cancer treatment, offering hope to countless patients.
The Challenge
However, immunotherapies often come with risks and challenges of their own:
- Side Effects: Checkpoint inhibitors can activate the immune system too strongly, leading to autoimmune-like conditions where healthy cells and tissues are mistakenly attacked.
- Limited Responders: Not all patients respond to checkpoint inhibitors or BiTEs, and predicting which patients will benefit remains a significant challenge.
- Cost: These therapies, especially newer modalities like BiTEs, can be prohibitively expensive, restricting access for many patients.
- Duration of Response: The duration of the response to checkpoint inhibitors can be variable, and for some patients, the effect is transient.
- Developmental Hurdles: The creation and refinement of checkpoint inhibitors and BiTEs demand a complex development process.
How DNA Origami Could Elevate Precision Medicine
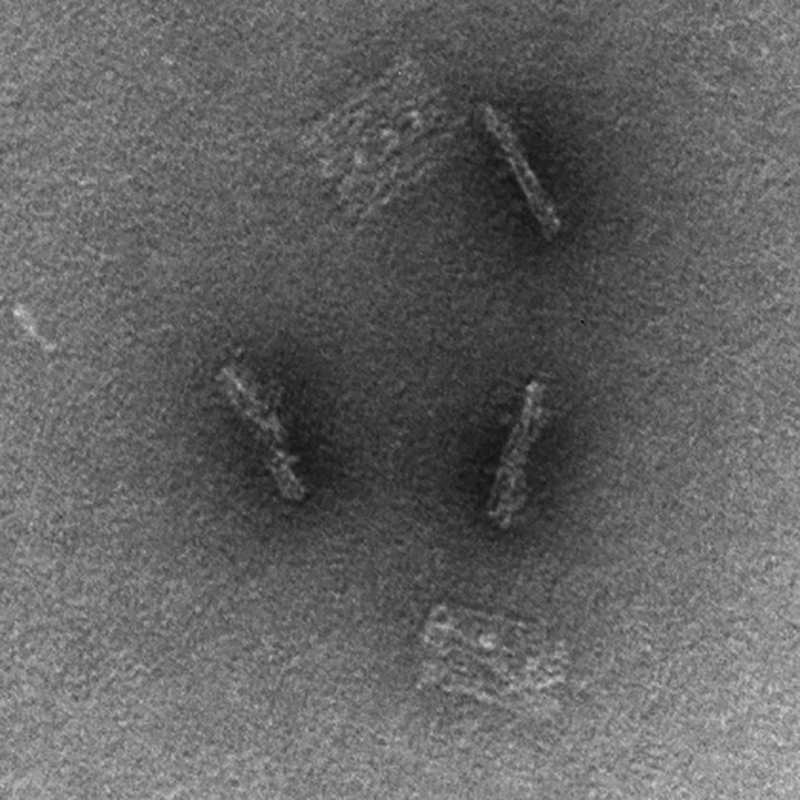
- Enhanced Therapeutic Delivery: DNA origami structures can serve as precise delivery vehicles, ensuring that treatments like CAR-T therapies or drugs reach their intended targets with minimal off-target effects.
- Customization at Its Best: With its high specificity, DNA origami can be tailored to address the unique genetic makeup of each patient, ensuring therapies are as effective as possible.
- Addressing Immunotherapy Challenges: DNA origami could be the answer to some of the current challenges faced by checkpoint inhibitors and BiTEs. By carrying molecules that modulate the immune response, the risk of adverse reactions could be significantly reduced; including engagement and activation of NK cells.
- Multifaceted Therapeutic Approach: Imagine a single DNA origami structure carrying multiple therapeutic agents and strategies, each designed to address different aspects of a disease. Such multi-pronged approaches could significantly improve therapeutic outcomes and reduce side effects; all in one delivery vehicle.
In essence, the convergence of DNA origami and precision medicine promises a future where treatments are not only more effective but also tailored to the intricate needs of each patient.
Conclusion: An Integrated Future
Precision medicine has come a long way, with CAR-T therapies, ADCs, and immunotherapies serving as the torchbearers of this revolution. Yet, these therapies are not without their challenges—challenges that DNA origami has the potential to address. As we stand at the cusp of the next big leap in healthcare, DNA origami could be the key to unlocking a future where treatments are not just personalized but also integrated, efficient, and exceptionally precise.
At DNA Nanobots we are experts in a field that is about to explode. If you have a therapeutic that you want delivered, we would love to help you do that. You provide the therapeutic, we provide the vehicle. Contact us at info@dnananobots.com or click below anytime.
by Patrick Halley, Co-Founder and CTO